Surfactant Protein A Human ELISA
Surfactant protein A (SP-A; surfactant- associated protein A – SFTPA; pulmonary surfactant- associated protein A – PSPA) is the major protein component of the lung surfactant in mammals. It belongs, together with SP-D, to the collectins’ family, due to its C-type lectin domain and the collagen-like N-terminal triple helix. The lectin domain mediates the interaction between a collectin and a wide variety of pathogens. The oligomeric structure of SP-A comprises two types of polypeptide chains: SP-A1 and SP-A2 transcribed from sftpa1 and sftpa2 genes. Six trimers of SP-A form its complete octadecameric structure. Human SP-A is expressed primarily in the lung, mostly in alveolar type II cells and also in non-ciliated bronchial epithelial cells. SP-A mRNA can be detected in fetal lung cells after only 20 weeks of gestation. SP-A has been found in various biological fluids, such as bronchoalveolar lavage fluid, sputum, serum, amniotic fluid and vaginal lavage fluid. It has also been found to be expressed in cells of the small and large intestine. SP-A is considered to be an important host defence components against respiratory allergens and pathogens. SP-A takes part in modulating the function of immune system cells – especially dendritic cells and T-cells. Many studies have shown that inflammatory mediators (e.g. TNF) are controlled by SP-A, both positively and negatively. Changes in SP-A production in the lung or its baseline concentrations in serum might be associated with progression or mortality at idiopatic pulmonary fibrosis (IPF). Reduced levels of SP-A in alveolar fluid were also reported in other pulmonary diseases, e.g. acute respiratory distress syndrome (ARDS). Furthermore, elevated levels of SP-A in lungs have been observed in pulmonary alveolar proteinosis (PAP).
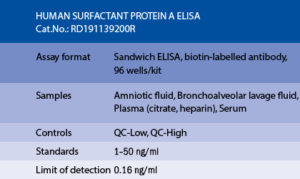
The RD191139200R Human Surfactant Protein A ELISA is a sandwich enzyme immunoassay for the quantitative measurement of human surfactant protein A in serum, plasma (citrate, heparin), bronchoalveolar lavage fluid and amniotic fluid.
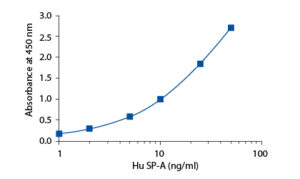
In the BioVendor Human Surfactant Protein A (SP-A) ELISA, standards, quality controls and samples are incubated in microplate wells precoated with monoclonal anti-human SP-A antibody. After 2 hours incubation at 37°C and washing, biotin labelled polyclonal anti-human SP-A antibody is added to the wells and incubated for 60 minutes with captured surfactant protein A. After another washing, streptavidin-HRP conjugate is added. After 30 minutes incubation and the last washing step, the remaining conjugate is allowed to react with the substrate solution (TMB). The reaction is stopped by addition of acidic solution and absorbance of the resulting yellow product is measured. The absorbance is proportional to the concentration of SP-A. A standard curve is constructed by plotting absorbance values against concentrations of standards, and concentrations of unknown samples are determined using this standard curve.
Intended use
Clinical Application
Test principle
Summary of protocol
– Emilsson OI, ORCID: http://orcid.org/0000-0002-7199-8491, Benediktsdottir B, Olafsson I, Cook E, Juliusson S, Bjornsson ES, Guethlaugsdottir S, Guethmundsdottir AS, Mirgorodskaya E, Ljungstrom E, Arnardottir ES, Gislason Thorn, Janson C, Olin AC. Respiratory symptoms, sleep-disordered breathing and biomarkers in nocturnal gastroesophageal reflux. Respir Res. 2016;17 (1):115
– Gargiulo P, Banfi C, Ghilardi S, Magri D, Giovannardi M, Bonomi A, Salvioni E, Battaia E, Filardi PP, Tremoli E, Agostoni P. Surfactant-derived proteins as markers of alveolar membrane damage in heart failure. PLoS One. 2014;9 (12):e115030
– Gaunsbaek MQ, Kjeldsen AD, Svane-Knudsen V, Henriksen ML, Hansen S. Surfactant proteins A, B, C and D in the human nasal airway: associated with mucosal glands and ciliated epithelium but absent in fluid-phase secretions and mucus. ORL J Otorhinolaryngol Relat S. 2014;76 (5):288-301
– Huttmann EM, Greulich T, Hattesohl A, Schmid S, Noeske S, Herr C, John G, Jorres RA, Muller B, Vogelmeier C, Koczulla AR. Comparison of two devices and two breathing patterns for exhaled breath condensate sampling. PLoS One. 2011;6 (11):e27467
– Liu HH, Chen CY, Chen GI, Lee LH, Chen HL. Relationship between indium exposure and oxidative damage in workers in indium tin oxide production plants. Int Arch Occup Environ Health. 2012 May;85 (4):447-53
– Malur A, Kavuru MS, Marshall I, Barna BP, Huizar I, Karnekar R, Thomassen MJ. Rituximab therapy in pulmonary alveolar proteinosis improves alveolar macrophage lipid homeostasis. Respir Res. 2012;13:46
– Podolanczuk AJ, Oelsner EC, Barr RG, Hoffman EA, Armstrong HF, Austin JH, Basner RC, Bartels MN, Christie JD, Enright PL, Gochuico BR, Hinckley Stukovsky K, Kaufman JD, Hrudaya Nath P, Newell JD Jr, Palmer SM, Rabinowitz D, Raghu G, Sell JL, Sieren J, Son. High attenuation areas on chest computed tomography in community-dwelling adults: the MESA study. European Respiratory Journal. July 2016;45 (2)
– Sterclova M, Vasakova M, Paluch P, Paulik M. Surfactant protein A in chronic extrinsic allergic alveolitis. Eur Respir J. 2012 Jun;39 (6):1543-4
– Susilovic-Grabovac Z, Banfi C, Brusoni D, Mapelli M, Ghilardi S, Obad A, Bakovic-Kramaric D, Dujic Z, Agostoni P. Diving and pulmonary physiology: Surfactant binding protein, lung fluid and cardiopulmonary test changes in professional divers. Respir Physiol Neurobiol. 2017 Apr 30;243:27-31. doi: 10.1016/j.resp.2017.04.012
– Vigh G, Erdey A. [Hereditoary keratosis palmaris et plantaris dissipatum Brauer]. Z Hautkr. 1977 Jan 15;52 (2):42-4

