TruQuick™ H.pylori Ag
H. pylori is a small, spiral-shaped bacterium that lives in the surface of the stomach and duodenum. It is implicated in the etiology of a variety of gastrointestinal diseases, including duodenal and gastric ulcer, non-ulcer dyspepsia and active and chronic gastritis.1, 2 Both invasive and non-invasive methods are used to diagnose H. pylori infection in patients with symptoms of gastrointestinal disease. Specimen-dependent and costly invasive diagnostic methods include gastric or duodenal biopsy followed by urease testing (presumptive), culture, and/or histologic staining.3 A very common approach to the diagnosis of H. pylori infection is the serological identification of specific antibodies in infected patients. The main limitation of serology test is the inability to distinguish current and past infections. Antibody may be present in the patient’s serum long after eradication of the organisms.4 HpSA (H. pylori Stool Antigen) testing is gaining popularity for diagnosis of H. pylori infection and also for monitoring the efficacy of the treatment of H. pylori infection. Studies have found that more than 90% of patients with duodenal ulcer and 80% of patients with gastric ulcer are infected with H. pylori.5 TruQuick H. pylori Ag is a rapid immunoassay for the qualitative detection of H. pylori antigens in feces specimens, providing results in ten minutes. The test utilizes antibodies specific for H. pylori antigens to selectively detect H. pylori antigens in human feces specimens.
- To collect fecal specimens: Collect sufficient quantity of feces (1-2 mL or 1-2 g) in a clean, dry specimen collection container to obtain maximum antigens (if present). Best results will be obtained if the assay is performed within 6 hours after collection. Specimen collected may be stored for 3 days at 2-8 C if not tested within 6 hours. For long term storage, specimens should be kept below – 20 C.
- To process fecal specimens:
- For Solid Specimens: Unscrew the cap of the Specimen Collection Tube then randomly stab the specimen collection applicator into the fecal specimen in at least 3 different sites to collect approximately 50 mg of feces (equivalent to 1/4 of a pea). Do not scoop the fecal specimen. •
- For Liquid Specimens: Hold the dropper vertically, aspirate fecal specimens, and then transfer 2 drops (approximately 80 μL) into the Specimen Collection Tube containing the Extraction Buffer. Tighten the cap onto the Specimen Collection Tube, then shake the Specimen Collection Tube vigorously to mix the specimen and the Extraction Buffer. Leave the tube alone for 2 minutes.
- Bring the pouch to room temperature before opening it. Remove the Test Cassette from the foil pouch and use it within one hour. Best results will be obtained if the test is performed immediately after opening the foil pouch. \
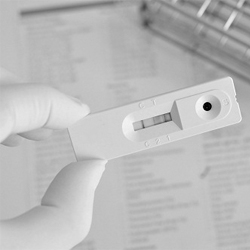
- Hold the Specimen Collection Tube upright and open the cap onto the Specimen Collection Tube. Invert the Specimen Collection Tube and transfer 2 full drops of the extracted specimen (approximately 80 μL) to the specimen well (S) of the Test Cassette, then start the timer. Avoid trapping air bubbles in the specimen well (S). See illustration below. \
- Read results at 10 minutes after dispensing the specimen. Do not read results after 20 minutes. Note: If the specimen does not migrate (presence of particles), centrifuge the extracted specimens contained in the extraction buffer vial. Collect 80 μL of supernatant, dispense into the specimen well (S) of a new Test Cassette and start afresh following the instructions mentioned above.
- Marshall BJ, McGechie DB, Rogers PAR, Glancy RG. Pyloric Campylobacter infection and gastroduodenal disease. Med J Australia 1985;149:439-44.
- Soll AH. Pathogenesis of peptic ulcer and implications for therapy. N Engl J Med 1990;322:909-16.
- Hazell SL, et al. Campylobacter pyloridis and gastritis I: Detection of urease as a marker of bacterial colonization and gastritis. Am J Gastroenterol 1987;82(4):292-96.
- Cutler AF. Testing for Helicobacter pylori in clinical practice. Am J Med 1996;100:35S-41S.
- Anand BS, Raed AK, Malaty HM, et al. Low point prevalence of peptic ulcer in normal individual with Helicobacter pylori infection. Am J Gastroenterol 1996;91:1112-1115.